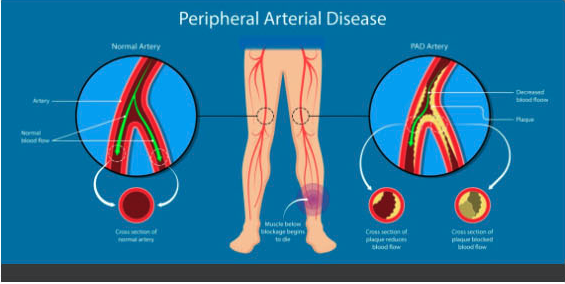
Peripheral Arterial Disease (PAD) is a disease resulting in blood flow reduction to the extremities and peripheral organs.
Unfortunately, PAD is an under-diagnosed disorder which mainly affects elderly although it can affect people at any age. About 15-20% of the people above the age of 65 are affected by PAD.
There are multiple risk factors for PAD including:
- Smoking cigarettes
- Diabetes Mellitus (DM)
- Hypertension
- Hyperlipidemia
The risk of PAD in smokers and diabetic patients is 4 and 2 times the normal population, respectively. PAD is an atherosclerotic disease. Atherosclerotic plaques consistent of cholesterol and calcium deposits will be formed inside the arteries and these plaques will grow over time and result in arterial occlusion which results in blood flow reduction in the affected limb.
What are the symptoms?
Although PAD can present with classic limb claudication but symptoms can be vague which emphasizes the need for taking a detailed history and careful physical exam in order to diagnose PAD. Patients may complain of leg cramps (claudication) which increases by walking and relieves by rest. Other symptoms include lower extremity discomfort or fatigue. Leg pain also increases by leg elevation and relieves by dangling of the legs at the bedside.
Checking the peripheral pulses are extremely important in order to diagnose PAD as diminished pulses are one of the earliest signs of PAD. Other signs include cold skin, skin discoloration or nonhealing ulcer.

How can PAD be diagnosed?
I order to diagnose PAD, it is better to start with noninvasive tests such as Ankle Brachial Index (ABI) and arterial Ultrasound (US)
In ABI, arterial systolic pressures are measured on both ankles and brachial arteries and by dividing the ankle to brachial systolic blood pressures, PAD can be diagnosed. ABI <0.9 is considered abnormal.
Arterial ultrasound is another modality to diagnose PAD. Arterial blood flow speed is measured during the arterial US and based on the blood flow velocity changes, severity and location of the PAD can be determined.
Arterial Computed Tomography Angiography (CTA) and Magnetic Resonance Angiography (MRA) are also great tools to diagnose PAD. They both provided the severity and location of the PAD which are extremely important for invasive procedure planning. When making the decision to order CTA vs MRA, we should consider the risks and benefits in each of these tests. In CT angiogram, patient is exposed to radiation and risk of contrast induce nephropathy and allergic reactions should be considered. On the other hand, MRA will not expose the patient to radiation or contrast induced nephropathy but expense can be an issue. MRA also can result in Gadolinum induced Nephrogenic systemic fibrosis (NSF) in patients with chronic kidney disease.
Finally, the gold standard test to diagnose PAD is invasive aortic angiogram with distal run off which is done in the cath lab under moderate sedation. This test is done by inserting an arterial sheath in the common femoral artery and taking pictures through catheters and using contrast under fluoroscopy. After taking pictures, arterial lesions can be treated using balloons or stents which will be discussed in our next blog post.